If you’re a runner, chances are you’ve heard of the condition that’s common to the sport called chondromalacia patella. You may know it as runner’s knee. You also may be intimately aware of the problems it can cause, since it puts a big dent in your running schedule. The symptoms of chondromalacia patellae, whether in one or both knees, mimic so many other painful conditions that can strike your knees. Seek medical attention from the best pain doctors at Pain Management NYC to get answers and relief.
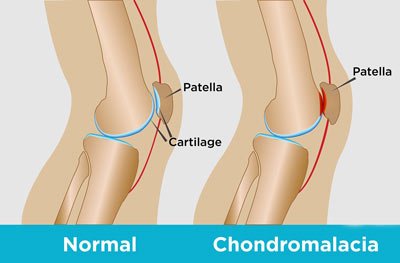
Under your kneecap, called the patella, rests a significant amount of cartilage that protects the bones from grinding against each other when your knee bends and pivots. As you age, this cartilage softens and breaks down. This is called chondromalacia patella. Without that protective cartilage, your shin and thigh bones begin rubbing together as you walk, exercise or bend your knee to pick something up off the floor.
When your bones rub together, the surrounding tissue becomes inflamed and causes pain. This inflammation can even push your kneecap slightly out of position, worsening the wear-and-tear of your cartilage and bones. That’s why you should see one of the best pain management doctors in Manhattan at Pain Management NYC at the first sign that something’s wrong. Your knees play a vital role in your everyday activities. Proper interventional chondromalacia patella treatment ensures you don’t have to suffer needlessly.
Risk Factors and Causes for Chondromalacia Patella
 While you age, some wear-and-tear in your joints is normal, but some individuals may be more at risk for dealing with chondromalacia patella. Runners are especially susceptible to chondromalacia patella, which is why the condition often is dubbed runner’s knee. Other risk factors include:
While you age, some wear-and-tear in your joints is normal, but some individuals may be more at risk for dealing with chondromalacia patella. Runners are especially susceptible to chondromalacia patella, which is why the condition often is dubbed runner’s knee. Other risk factors include:
- Having had a previous knee injury, such as a fracture, dislocation, or other injury
- Being overweight, which puts additional stress on your knees
- Playing high-impact sports or participating in a hobby that involves repetitive motions of your knees, such as soccer players, cyclists and tennis players
- Having flat feet
Interestingly, active young people, especially females, are more susceptible to the condition because they have less muscle mass to protect the complex knee joints. Pain can be caused by the abnormal position of your kneecap, repetitive motions and weakness or tightness of the muscles around your knee. These all contribute to excessive wear-and-tear that can result in chondromalacia patella.
Symptoms Requiring Chondromalacia Patella Treatment
The symptoms associated with chondromalacia unfortunately mimic other knee problems, which is why you need to be diagnosed and treated by our doctors. Common symptoms that often accompany chondromalacia patellae include:
- A grinding feeling and sound when your knees flex for any reason, such as traversing stairs, exercising or standing after being seated for a while
- A dull, achy pain that can be focused behind or below your kneecap or somewhere down the sides of the knees
- Swelling and inflammation, much like that of arthritis
- A vague sense of discomfort in the inner front section of your knee
- Tightness in and around your knee
Left untreated, this knee condition can cause your quadriceps to lose strength and seem to give out when you least expect it. Don’t let that happen. Visit Pain Management NYC for diagnosis and treatment.
Diagnosing Chondromalacia Patella
Your nationally recognized pain doctor checks your gait, watches how you hold your weight and looks for abnormalities as you bend your knee. He asks questions regarding your medical history and past injuries, and he may also want to know about your exercise habits and sleeping conditions.
After completing the physical exam, your doctor may wish to either get a better picture of your kneecap and surrounding tissue to rule out the possibility of growths or infection. He may order blood tests or imaging scans such as an MRI. Occasionally, it may be necessary to perform an arthroscopy, using a tiny camera inserted into your knee to better view what might be causing your pain.
Chondromalacia Patella Treatment
As with most treatment plans, less is sometimes more. Ideally, your doctor wants to be able to treat your chondromalacia patella with interventional treatment like rest and activity modification, all while managing your current pain. But various forms of treatment are available, including:
- Ice packs placed on the knee for 20 minutes at a time, several times a day, to reduce inflammation
- Elevating your knee to reduce the swelling that increases discomfort
- Over-the-counter or prescription pain relievers
- Topical pain medications
- Advice about different methods of exercise, such as swimming, to relieve pressure on your knees
- Losing weight
- Compression bandages or braces
- Supportive shoes or inserts
- Injections to give you relief so that you can participate in other healing therapies
If conservative methods aren’t successful, minimally invasive arthroscopic surgery may be able to fix anatomical abnormalities or remove any small pieces of bone or cartilage that may have worked loose. Your procedure is followed by multidisciplinary rehabilitation for pain. Rarely, more extensive surgical intervention may be required.
Correctly diagnosing and finding the best chondromalacia patella treatment options for your lifestyle and needs is the goal of regenerative treatment as practiced by the best pain management doctors in Midtown. Get the help you need to get out of pain; contact Pain Management NYC today.

