Sometimes, taking risks like rock climbing and car racing leads to hard falls or accidents that end with fractures in your pelvic bones or tears in the soft tissues surrounding your pelvis. Diseases that cause poor immunity or weak bones can also lead to pelvic fractures. These can then lead to nerve pain and the need for pudendal neuralgia treatments. New treatments for pudendal neuralgia are available at Pain Management NYC. Call them the minute you feel pain in your pelvis to avoid further complications.
What Is Pudendal Neuralgia?
Pudendal neuralgia is a chronic condition that affects the pudendal nerve, which runs from your lower back to your genitals and anus. It causes pain, numbness, tingling and burning sensations in your pelvic area, affecting your quality of life and sexual functioning.
Pudendal neuralgia has various causes, such as:
- Nerve compression
- Trauma
- Errors made in surgery
- Infection
Pudendal neuralgia is also associated with other conditions, such as endometriosis, pelvic inflammatory disease and interstitial cystitis. Pain Management NYC has a team of experienced and compassionate doctors who offer the best pudendal neuralgia treatment in NYC.
These pain experts use a multidisciplinary approach that combines medication, nerve blocks, physical therapy and minimally invasive procedures to relieve your pain. They also provide personalized care and support to help you cope with the emotional and psychological aspects of pudendal neuralgia.
What Causes Pudendal Neuralgia?
Pudendal neuralgia occurs when the pudendal nerve is damaged, irritated or compressed. The pudendal nerve is a major nerve that runs from the lower back to the pelvic area, where it branches off into smaller nerves that supply sensation and movement to the genitals, anus and perineum. The pudendal nerve also controls the sphincter muscles that help you urinate and defecate. Pudendal neuralgia can occur without a clear cause, in which case it’s called idiopathic pudendal neuralgia.
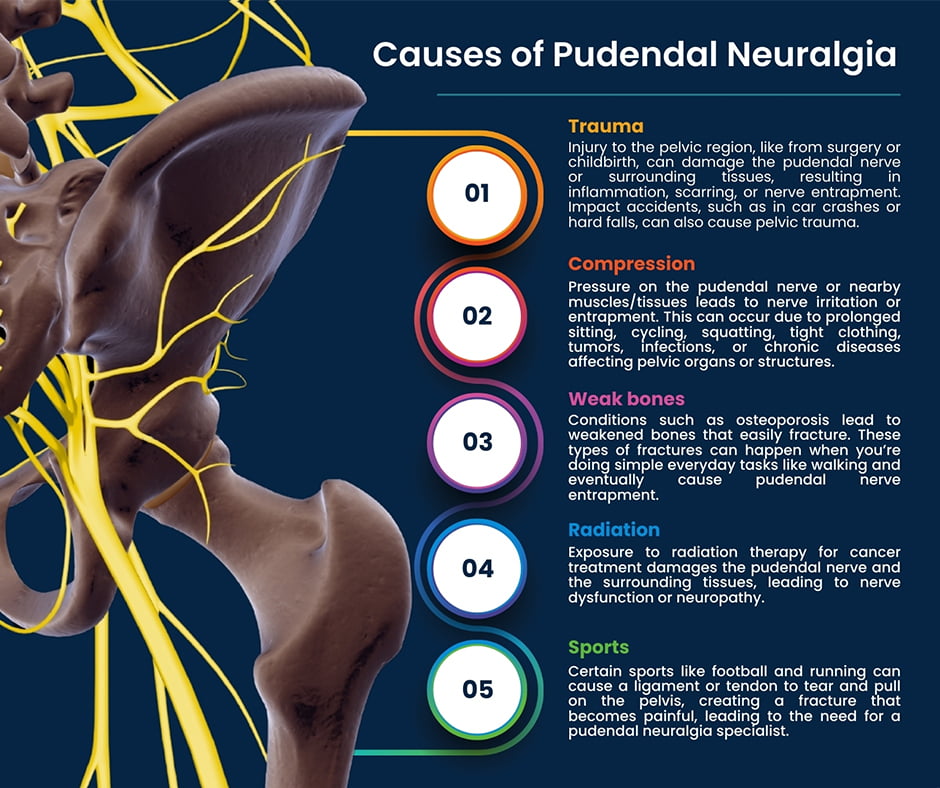
However, there are several possible causes of pudendal neuralgia, including:
- Trauma. Injury to the pelvic region, such as from surgery or childbirth, damage or stretch the pudendal nerve or the surrounding tissues. This results in inflammation, scarring or entrapment of the nerve. Impact accidents such as you might experience in a car accident or a hard fall can cause pelvic trauma.
- Compression. Pressure on the pudendal nerve or the nearby muscles or tissues causes nerve irritation or entrapment. This happens due to prolonged sitting, cycling, squatting or wearing tight clothing. It’s also caused by tumors, infections or chronic diseases that affect the pelvic organs or structures.
- Weak bones. Conditions such as osteoporosis lead to weakened bones that easily fracture. These types of fractures can happen when you’re doing simple everyday tasks like walking and eventually cause pudendal nerve entrapment.
- Radiation. Exposure to radiation therapy for cancer treatment damages the pudendal nerve and the surrounding tissues, leading to nerve dysfunction or neuropathy.
- Sports. Certain sports like football and running can cause a ligament or tendon to tear and pull on the pelvis, creating a fracture that becomes painful, leading to the need for a pudendal neuralgia specialist.
What Are the Risk Factors for Pudendal Neuralgia?
Pudendal neuralgia, though rare, is a condition that can affect anyone, but some factors increase your risk of developing it. One of them is age. Pudendal neuralgia is more common in adults older than 19, and the risk increases with age as the nerve and the surrounding tissues degenerate or become less flexible. Another risk factor is gender. Pudendal neuralgia affects both men and women, but women are more prone to it due to hormonal changes, pregnancy, childbirth and pelvic surgeries.
Other risk factors include:
- Physical activity. Certain activities that put pressure or strain on the pudendal nerve or the pelvic region trigger or worsen pudendal neuralgia.
- Medical conditions. Some diseases or disorders that affect the pelvic organs and structures cause inflammation, infection or compression of the pudendal nerve. These include endometriosis, pelvic inflammatory disease, interstitial cystitis, prostatitis and tumors, as well as other chronic diseases.
What Are the Long-Term Consequences of Untreated Pudendal Neuralgia?
Pudendal neuralgia has long-term effects on physical, mental and emotional health. Since pain is the primary symptom of untreated pudendal neuralgia, consequences have a devastating impact on your overall health and well-being, so seek medical help as soon as possible. Early diagnosis and treatment prevent further complications and improve your prognosis.
If left untreated, pudendal neuralgia leads to:
- Chronic pain. The pain caused by pudendal neuralgia becomes constant and unbearable, interfering with your daily activities and reducing your quality of life. Chronic pain also causes depression, anxiety, insomnia and fatigue.
- Sexual dysfunction. Pudendal neuralgia makes having sex painful, difficult or impossible, affecting your sexual satisfaction and intimacy with your partner. It also interferes with arousal, orgasm and erectile function.
- Urinary and bowel dysfunction. Pudendal neuralgia affects your ability to control your bladder and bowel movements, causing incontinence, urgency, frequency and retention issues. These symptoms are embarrassing, inconvenient and uncomfortable.
- Nerve damage. Pudendal neuralgia causes permanent damage to the pudendal nerve and the surrounding tissues, resulting in nerve dysfunction or neuropathy. This causes numbness, weakness or paralysis in the pelvic area, affecting your sensation and movement.
- Cauda equina syndrome. In rare cases, pudendal neuralgia may mimic symptoms of the cauda equina, a bundle of nerves at the lower end of the spinal cord. This is a medical emergency that causes severe pain, numbness, weakness or paralysis in the lower body, as well as loss of bladder and bowel control. If not treated promptly, cauda equina syndrome causes permanent disability or even death.
Where Can I Find a Pudendal Neuralgia Specialist Near Me?
Pain Management NYC doctors offer new treatments for pudendal neuralgia. They work with you to find the best pudendal neuralgia treatment in NYC that suits your needs and preferences. They also monitor your progress and adjust your treatment plan as needed.
Your doctor may prescribe medication to reduce inflammation, relax your muscles or block the nerve signals that cause pain. These may include anti-inflammatory drugs, muscle relaxants, antidepressants, anticonvulsants or opioids. You may also use topical creams or patches to numb the affected area.
Other treatments include:
- Nerve blocks. A nerve block is an injection of local anesthetic and steroid medication into or near the pudendal nerve. This provides temporary relief from pain and inflammation and helps diagnose the source of your nerve problem.
- Physical therapy. A physical therapist teaches you exercises to relax and stretch your pelvic floor muscles and other muscles that irritate the pudendal nerve. They also use techniques such as massage, heat, cold and electrical stimulation to ease pain and improve blood flow.
- Lifestyle changes. Your pudendal neuralgia specialist recommends changes to your daily habits when necessary to reduce the pressure on your pudendal nerve. These include avoiding prolonged sitting, cycling, squatting or wearing tight clothing, using a cushion or a donut pillow when sitting and practicing good posture and hygiene.
- Surgery. Surgery is usually the last resort for pudendal neuralgia treatment and only considered when other treatments have failed, or the nerve is severely damaged. Surgery involves decompressing, releasing or repairing the pudendal nerve, or cutting the nerve to stop the pain signals.
Contact Pain Management NYC for the best pudendal neuralgia treatment in NYC, using a combined approach. Don’t let pudendal neuralgia ruin your life when there’s a pudendal neuralgia specialist near me so close in New York City.

Leon Reyfman, MD, is a top-rated, best-in-class interventional pain management doctor. He is a nationally recognized pain relief specialist and is among the top pain care doctors in New York City and the country. He is an award-winning expert and contributor to prominent media outlets.
Dr. Leon Reyfman has been recognized for his thoughtful, thorough, modern approach to treating chronic pain. He has been named a “top pain management doctor in New York” and one of “America’s Top Doctors™” for advanced sports injury treatments. Among other accolades, he was voted by peers as a “Castle Connolly Top Doctors™” and “New York Super Doctors™”. Dr. Leon Reyfman was a part of the medical team at the 2016 Summer Olympic Games in Rio de Janeiro, Brazil.
