Our feet undergo a lot of stress every day, and occasional aches and pain are normal. However, stabbing heel pain in the morning, a recurring ache that comes on after activity and sticks around for days, or a new, painful bump on the back of your heel are causes for concern and need medical attention. At Pain Management NYC, Dr. Leon Reyfman and his team can help you determine why your heel hurts and what may be causing this pain. With his latest non-surgical and surgical options and quality care, he provides lasting pain relief for your heel and foot conditions.
Heel pain is common among men and women and usually occurs after repetitive stress on the heel, such as long-distance running or structural issues with the bones and soft tissues. If you ignore this pain and do not get it treated, you may develop foot problems that require intense treatment and longer recovery. The good news is that heel pain rarely needs surgery.
Where Does Heel Pain Develop?
 Heel pain occurs under the heel or just behind it, where the Achilles tendon connects to the heel bone. Sometimes, it can affect the side of the heel, or you may feel pain within the heel bone itself. You might experience pain, soreness, or tenderness anywhere in the heel due to inflammation, bone changes, and nerve compression. Heel pain is a sign that your heel needs healing.
Heel pain occurs under the heel or just behind it, where the Achilles tendon connects to the heel bone. Sometimes, it can affect the side of the heel, or you may feel pain within the heel bone itself. You might experience pain, soreness, or tenderness anywhere in the heel due to inflammation, bone changes, and nerve compression. Heel pain is a sign that your heel needs healing.In most cases, heel pain resolves without treatment. But when you continue activity despite a sore heel, the pain worsens, and it could lead to a chronic condition with additional symptoms. Timely care and proper treatment restore your freedom of movement and give you a chance to enjoy a pain-free life.
Read on to learn about the top causes of heel pain and what you can do to ease this discomfort.
Top Causes of Heel Pain
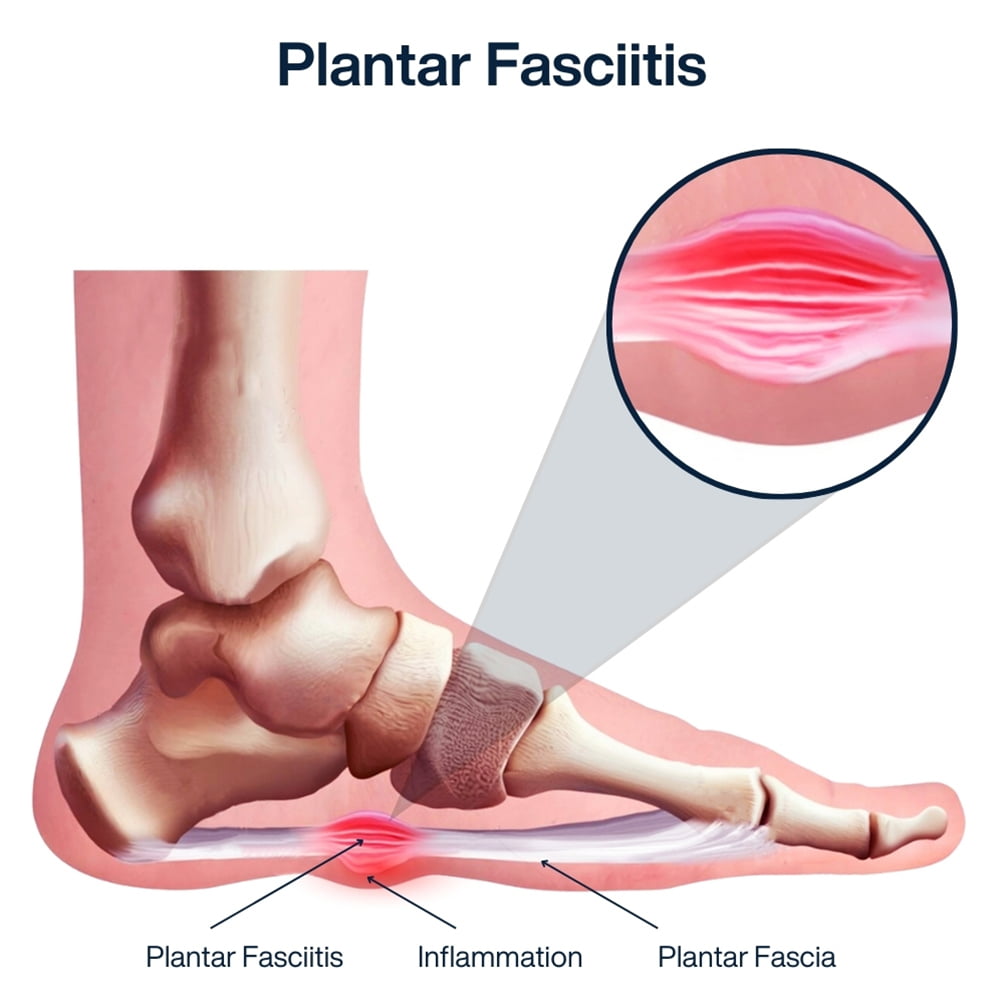
Plantar Fasciitis – The Most Common Cause of Heel Pain
Pain that occurs under the heel is known as plantar fasciitis. It is the most common cause of heel pain. The plantar fascia is a strong, thick ligament that runs from the heel bone to the tip of the foot. When the fascia is stretched too far, its fibers become inflamed, resulting in pain. The pain usually occurs where the ligament attaches to the heel bone, but it can be felt in the middle of the foot too.
This condition usually occurs due to repetitive motion or anything that puts a lot of pressure on the arch of the foot. Runners and people who wear shoes without proper support often face this problem. Structural foot problems such as high arches or flat feet or wearing shoes without adequate arch support can also lead to plantar fasciitis.
When and Where Does Your Heel Hurt With Plantar Fasciitis?
Planter fasciitis pain can flare up at any time. Some people feel pain in their heel during or after exercise, while others experience it after being on their feet for a long time. If your heel pain occurs after walking or other exercise, you will feel a sharp, stabbing pain in the arch of the foot or the bottom of the heel. It is a sign that plantar fascia is inflamed or damaged from overuse and needs care.
One of the most common signs of plantar fasciitis is heel pain after long periods of rest, especially when you wake up in the morning. The way you rest your foot in the bed may cause the foot muscles to tighten. You can feel this tightness as you lie in the bed, and when you put your foot on the ground, you will feel the worst kind of pain.
It is the same reason you will also experience heel pain after sitting for a while. Getting up and walking a bit stretches the tissue out and eases the pain.
Diagnosing and Treating Plantar Fasciitis
Your healthcare provider or pain management doctor can diagnose plantar fasciitis after examining your foot carefully and analyzing your pain symptoms. Several at-home treatments help keep the inflammation down and manage pain effectively. They include hot and cold therapy, ample rest, targeted stretches and exercises, as well as getting more supportive footwear.
Specialists recommend avoiding going barefoot, even at home. It is because lack of footwear puts additional strain on your feet. Slipping on supportive shoes or slippers can keep your muscles relaxed, and prevent pain. If your heel pain does not improve or begins to impact routine activities, your doctor may prescribe a cortisone injection. Surgery is also an option if conservative treatments do not work.
Other Causes of Heel Pain
Several other problems can cause pain to develop at the back of the heel. They include:
Achilles Tendonitis
If you are experiencing pain above the heel or at the back of your ankle during and after activity, it may be Achilles tendinitis. The Achilles tendon is a fibrous tissue that connects the calf muscle to the heel bone. It enables you to walk, run, jump, or push up on your toes. It is the body’s longest and strongest tendon. Overuse or injury can inflame the tendon, resulting in pain, swelling, and stiffness in the back of the heel.
Mostly runners and basketball players suffer from Achilles tendonitis due to tissue overuse injury, particularly when they increase the intensity or duration of their workouts. It also affects people who only participate in sports occasionally. When stretched beyond its normal range, the Achilles tendon develops multiple microscopic tears. It thickens, weakens, and becomes painful at the back of the heel. You may also experience limited range of motion as you flex your foot.
Signs of Achilles tendonitis include a mild ache that gets more intense with continued activity as well as tenderness or stiffness after working out or long periods of rest. However, the pain usually improves with mild activity and stretching throughout the day.
As with other overuse injuries, the best treatment for Achilles tendonitis is rest and avoiding or modifying activities to reduce strain. Your top pain specialist may also recommend additional treatments such as physical therapy, wraps, braces, or splits to keep the pain down and help the tendon heal. If you have tears in your Achilles tendonitis, surgery becomes necessary.
Haglund’s Deformity
Haglund’s deformity is a condition with a bony section on the back of the heel. The soft tissue near the Achilles tendon becomes irritated as the bony enlargement constantly rubs against the shoes.
Haglund’s deformity is often called the pump bump because it is common among women who wear high heels. It affects the heel bone and the surrounding soft tissue. However, any shoes with a rigid back, including men’s shoes and ice skates, can also put pressure on the back of the heel, causing irritation and inflammation. The pain may cause you to limp, and can also cause swelling and tenderness around the heel.
Symptoms of Haglund’s deformity include:
- Pain in the area where the Achilles tendon attaches to the heel
- Swelling at the back of the heel
- Redness and inflammation on the back of the heel
The best way to relieve pain is by wearing shoes that have soft backs. Taking over-the-counter anti-inflammatory medications and icing your heel also eases pain and swelling. Call your doctor if your heel pain does not subside as Haglund’s deformity can lead to another painful condition, called bursitis, if it is not treated timely.
Heel Bursitis
Bursitis is inflammation of the bursa, a small fibrous sack full of fluid at the back of the heel that cushions the bones, ligaments, and muscles. The bursa lubricates areas where the tissues rub against each other, allowing fluid movement. Direct pressure or repetitive motion, such as landing awkwardly or hard on the heels, excessive pressure from footwear, or spending a lot of time on your feet, causes these sacs to become inflamed and swell.
You may have a tender, bruise-like feeling deep inside the heel or at the back of the heel, and sometimes your Achilles tendon may swell as well. The pain usually gets worse as the day goes on. You have bursae (plural of bursa) throughout your body, both in and on the joints, that are at risk of rubbing and creating pressure.
There are two types of heel bursitis, and they are related to the locations of specific fluid pockets.
Subcalcaneal bursitis – The calcaneal bursa is located between the Achilles tendon and the skin at the back of the heel. Calcaneal bursitis is often linked to Haglund’s deformity, and it comes from wearing shoes that dig into the back of the heel. Women who wear high heels or athletes who wear shoes with the wrong fit are at higher risk for this type of inflammation. You may have calcaneal bursitis if you have pain, redness, and swelling on your heel that makes it hard to put on your shoes.
Retrocalcaneal bursitis – The retrocalcaneal bursa is located between the heel bone and the Achilles tendon, just above where the Achilles tendon meets the heel bone. This type of bursitis happens after repeated irritation of the bursa. It may be related to Achilles tendonitis and Haglund’s deformity and is common in people with posterior calcaneal bone spurs, which may need surgical removal. Severe pain and swelling where the Achilles tendon joins the heel bone is a sign of retrocalcaneal bursitis.
Rest, anti-inflammatory medications, and applying heat or ice packs help to treat bursitis. It is necessary to avoid activities that worsen pain, such as wearing ill-fitting footwear and a jog in the park. Call your doctor if your heel pain does not go away after at-home remedies or if your heel is hot to the touch.
Heel Fracture
Injury, repetitive stress, strenuous exercise, sports, or heavy manual work can fracture the large bone of your heel called the calcaneus. Sometimes, fractures happen suddenly following a traumatic event, while at other times, a heel fracture develops more slowly as a result of overuse.
Runners are at a high risk of a stress fracture in the metatarsal bones of the foot. Osteoporosis, a condition that causes bones to weaken, can also cause stress fractures.
Calcaneus fractures – Calcaneus fracture occurs following a traumatic event, such as after a fall or jump from a great height or in a car accident, and causes sudden, intense pain in the heel. Your doctor will do a physical examination, take X-rays to determine the severity of the problem and recommend the best treatment.
Stress fracture – Stress fractures that result from overuse begin with a small hairline fissure in the bone. This pain comes slowly and depends on the location and severity of the fracture. Most people with stress fractures experience heel pain when they walk, but it may not go away even at rest. The pain is usually more manageable in the morning and worse at night.
Avoiding physical activity and restricting the weight placed on the heel is essential if you have a stress fracture. If left untreated, the pain will become more severe and may lead to a complete fracture.
The Most Uncommon Cause of Heel Pain – Plantar Bone Spurs
If plantar fasciitis is not treated, it can cause calcium deposits on the heel bone, and create bone-like growths called planter bone spurs, or heel spurs. Long-term repetitive straining of the ligaments that connect the heel to the toes can lead to a bony protrusion on the underside of the heel bone.
These bony growths form as your foot tries to heal itself. Heel spurs are often painless, but some people may experience pain. If you are having heel pain, it is more likely from another condition like plantar fasciitis.
When to See a Doctor?
If your heel pain continues for more than 2 weeks and persists even when you are not standing or walking, it is time to pay attention and seek medical help. Call your doctor if you are having:
- Severe pain with swelling near the heel
- Pain, numbness, or tingling in the heel, as well as fever
- Difficulty walking as usual
- Difficulty bending the foot downward or tiptoeing
Getting help for heel pain is a step in the right direction. Your doctor will identify the causes behind your discomfort and suggest the best ways to treat heel pain at home, including rest, ice or heat therapy, and light exercises and stretches.
If your pain is resulting from some foot or heel condition, they prescribe pain medications, therapies, and advanced care to help you feel better.
Discomfort in your feet can make it very difficult to get around and perform your routine activities. Whatever the cause of your heel pain, Dr. Leon Reyfman has the expertise and experience to provide you with an accurate diagnosis and effective treatment. Call Pain Management NYC and schedule an appointment with our board certified specialist to find quick relief from your heel pain. He recommends the best treatment options that restore your freedom of movement and get you back on your feet as soon as possible.

Boleslav Kosharskyy, MD, is a top-rated, best-in-class interventional pain management doctor. He is board-certified in Anesthesiology, Interventional Pain Medicine, and Palliative Care.
Dr. Kosharskyy is an Associate Professor of Anesthesiology and Rehabilitation Medicine at Albert Einstein Medical College. He’s also the Associate Medical Director of Pain Medicine and Director of Anesthesia for the Joint Replacement Center at Montefiore Medical Center and Albert Einstein Medical College.
He is an active member of the American Society of Anesthesiology (ASA), the American Society of Regional Anesthesia and Pain Medicine (ASRA), and the New York State Society of Anesthesiologists (NYSSA)
